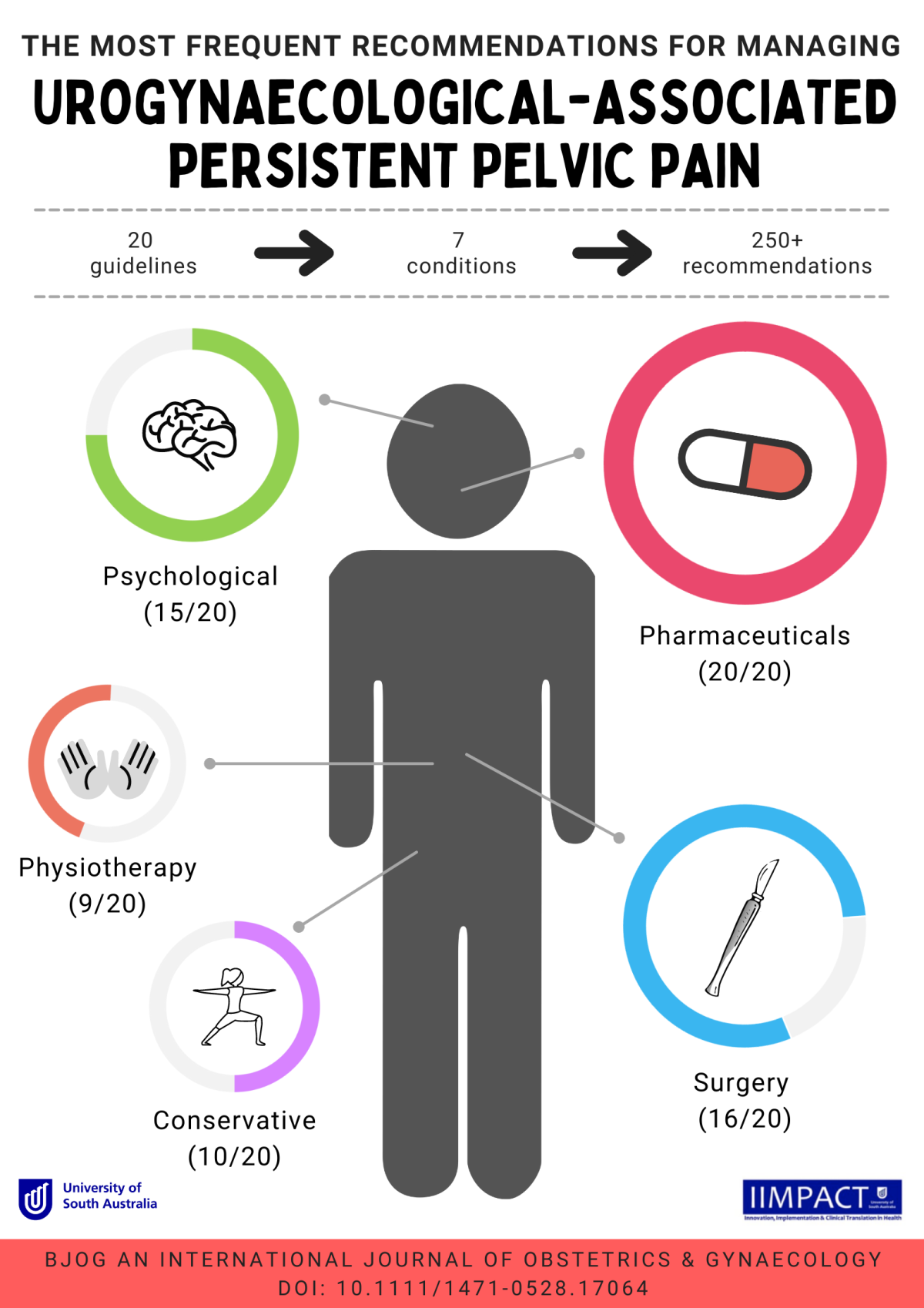
Persistent Pelvic Pain (PPP) is an umbrella term for a variety of complex conditions. Those conditions are impacted by biological, psychological, and social factors; therefore, many treatment options are used to manage PPP. Clinical practice guidelines (CPGs) are used to help improve the quality and consistency of diagnosis and treatment. Unfortunately, there are disparities between guidelines about what is considered best practice of care. The team at UniSA IIMPACT in Health, Persistent Pain conducted a systematic review to discover what treatment options are most recommended in PPP guidelines and to evaluate the quality of those recommendations. These results can help determine the appropriateness of treatments for PPP in clinical practice.
What guidelines are out there?
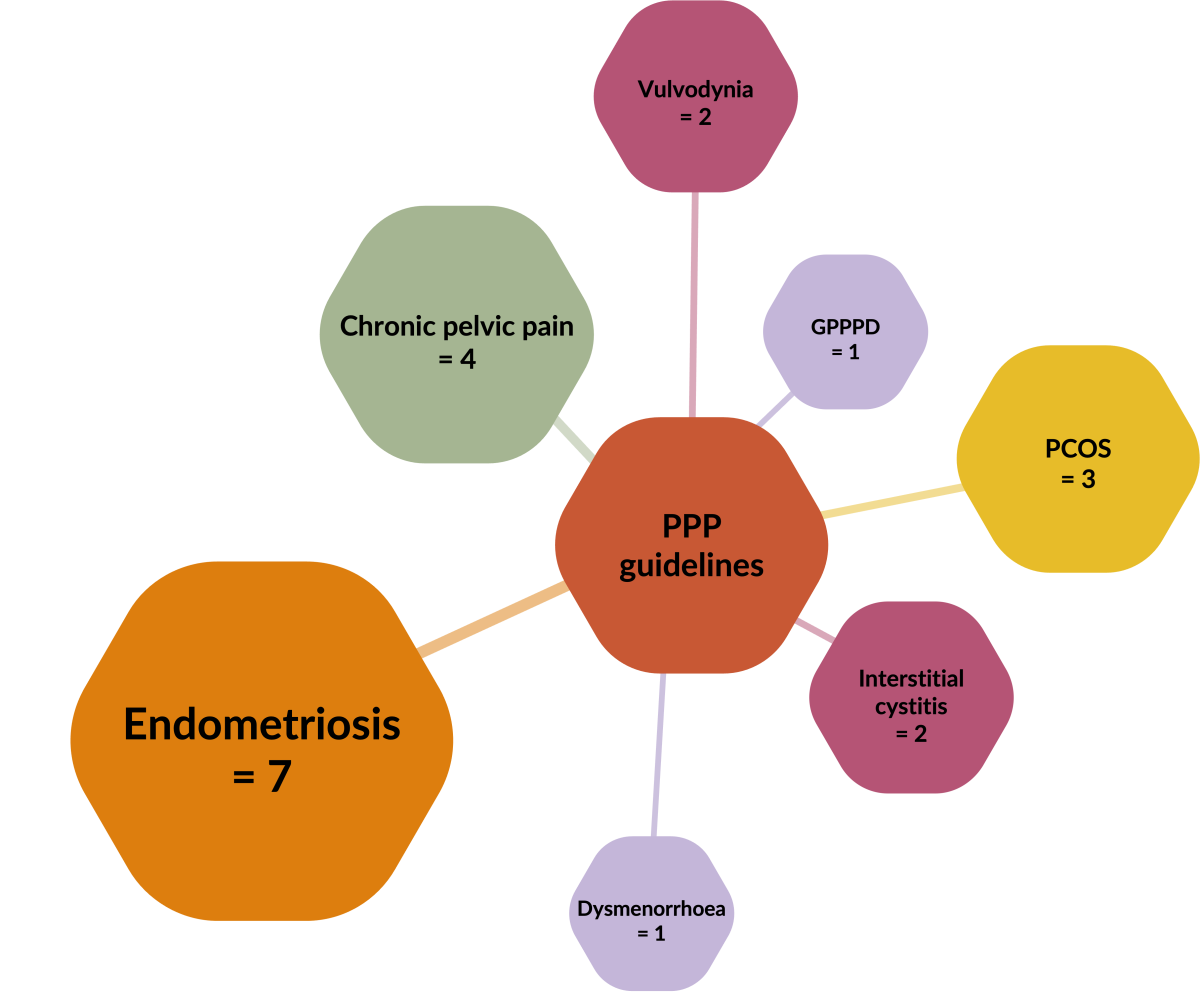
We discovered 20 CPGs for seven urogynaecological PPP conditions, including endometriosis, chronic pelvic pain, polycystic ovarian syndrome (PCOS), vulvodynia, interstitial cystitis, dysmenorrhoea, and genito-pelvic pain/penetration disorder (GPPPD).
What do PPP guidelines recommend?
All 20 PPP CPGs recommended the use of pharmaceutical interventions, most commonly hormonal therapies (15) and analgesics (12). Hormonal therapy recommendations were supported predominately by ‘high’ to ‘moderate’ levels of evidence, and most recommendations for analgesics were based on expert opinion (lowest level of evidence).
Most CPGs also recommended surgical interventions (16/20) and the most frequent were for hysterectomy (10) and laparoscopy (9). However, for endometriosis, hysterectomy was often recommended by expert opinion and laparoscopy was often supported with low-quality evidence.
Although many (15/20) CPGs recommended psychology, they were often vague and non-specific. Few (9/20) CPGs recommended physiotherapy as part of PPP management. For those that did, biofeedback and manual therapy were most common. Half of the CPGs recommended conservative interventions. The most common were for dietary changes and acupuncture , which were supported predominately with low levels of evidence.
Where to now?
Although guidelines recommend a variety of treatments for PPP, this review highlights the lack of high-quality research backing up those recommendations. Improving the quality of the evidence base will not only guide clinical decision making but will likely lead to improved patient outcomes. We should consider expanding the scope of PPP guidelines to explore recommendations for multidisciplinary management, which is common in clinical practice. It would also be beneficial for endometriosis guidelines to reconsider what currently appears to be an outdated ‘biomedical’ approach to pain management (surgery and medical interventions). Addressing these research and practice gaps is pivotal to improving care for people with PPP.
 Skip to main content
Skip to main content