There are no quick fixes in managing endometriosis and chronic pelvic pain. A therapeutic relationship is likely to entail repeated visits, individualised care and a multidisciplinary approach that changes over time. People with endometriosis can access a chronic care plan for allied health services.
Referrals to physiotherapists, dietitians, psychologists, pain specialists, surgeons, gastroenterologists and fertility specialists may be required at different times in the treatment course. We have provided some ideas for recommended guidelines and pain treatments to consider when formulating your treatment plan.
Treatment guidelines for endometriosis
A recent systematic review evaluated the clinical guidelines for the management pf persistent pelvic pain and recommended the following guidelines:
Managing pain
We know chronic pain is complex, here are some suggestions for managing pain.
Treatments for reducing pain triggers
| Option 1: Menstrual suppression | Option 2: Surgical removal of lesions |
|---|---|
| Continuous COC | 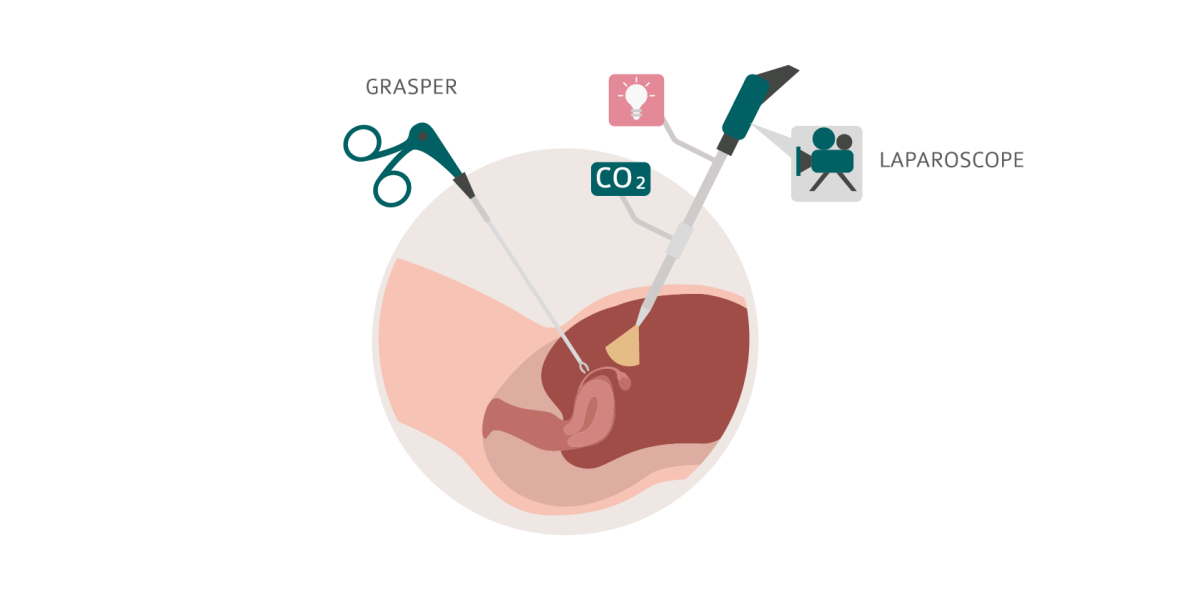 |
| Progestogens (oral, implant, IUD) | |
| GnRH agonists | |
| GnRH antagonists | |
| Selective progesterone receptor modulators | |
| Weak androgens |
Treatments for pelvic organ (visceral) sensitisation
| NSAIDs |  |
| FODMAP diet | |
| Regular bladder emptying | |
| Lubrication with sex/sexual aids (e.g. OHNUT) | |
| Neural modulators | |
| Gastroenterologists / urologists | |
| Dietitians/nutritionists |
Treatments for pelvic muscle (somatic) sensitisation
| Pelvic floor physiotherapy |  |
| PR diazepam (acute spasm) | |
| Topical amitriptyline | |
| Botox | |
| Neural modulators | |
| Pain specialists |
Treatments for cerebral cortex (central) sensitisation
| Acetaminophen (paracetamol) |  |
| Serotonin and norepinephrine – reuptake inhibitors | |
| Behavioural modifications | |
| Self care / mindfulness | |
| Pain specialists | |
| Counsellors / psychological support | |
| Neurologists |
When should I refer to a specialist gynaecologist?
Knowing when to refer your patient to a specialist gynaecologist can make all the difference to a person's experience with endometriosis and chronic pelvic pain. Below is a quick guide to determine when you may want to refer:
- When hormonal treatments and simple analgesics are not managing pain
- If the patient is needing to take time off work or school regularly because of pelvic pain
- When a transvaginal scan or MRI shows endometriosis
- When imaging is negative but pain symptoms persist
- If ovarian reserve as measured by anti mullerian hormone or antral follicle count on a scan is low
- When there is pain with intercourse or tenderness at the top of the vagina
 Skip to main content
Skip to main content