Laparoscopy is a surgical procedure where a thin telescope is placed into the abdomen to magnify the tissues and see even small amounts of endometriosis on the organs. It is now agreed that endometriosis can be diagnosed without laparoscopy but it is still recommended if no endometriosis was detected with ultrasound or MRI.
What is a laparoscopy and why do I need one?
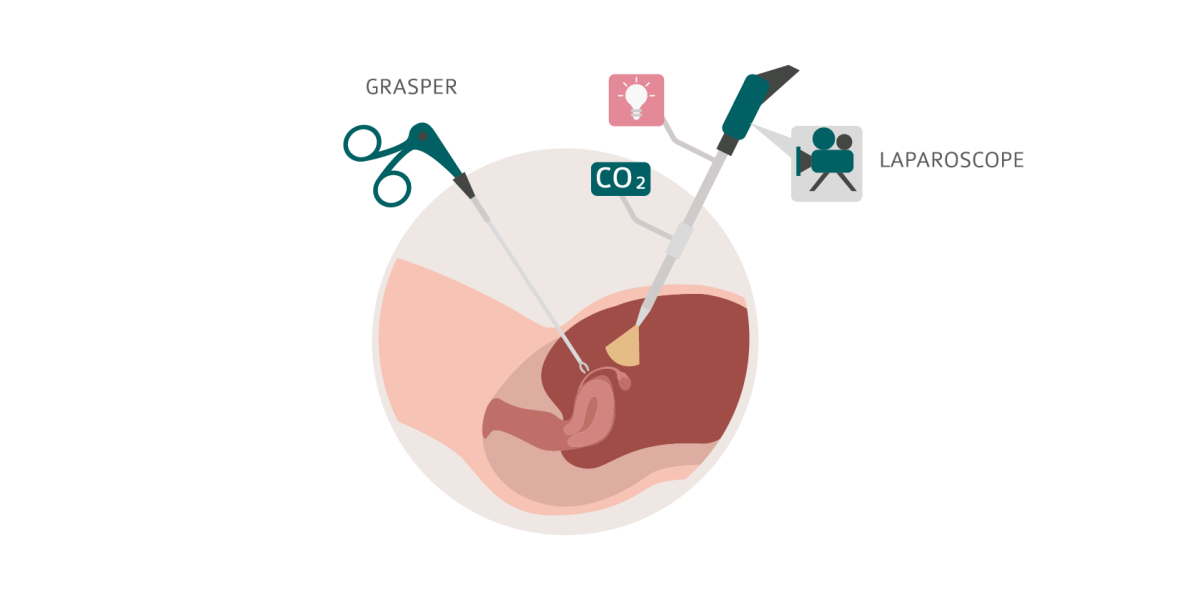
Laparoscopy is the most common surgery to diagnose and treat endometriosis. It is a surgical procedure where a thin telescope is placed into the abdomen to see the organs of the abdomen and pelvis. A laparoscopy can magnify the tissues and even small amounts of endometriosis can be seen. Areas where endometriosis may be present are cut out or vaporised at the time of the laparoscopy. When tissue is cut out, it can be sent to a pathologist to be viewed under a microscope to confirm the diagnosis. The location of the endometriosis may be close to organs, blood vessels and nerves and this may require other surgery to completely remove the disease. This is most commonly done at the same time as the laparoscopy.
The usual location for the laparoscope to be placed is through the umbilicus (belly button). The size of the hole needed is only 1cm or less (about the size of your little finger nail). During the laparoscopy, other instruments may be inserted using very small holes into the abdomen to help facilitate the surgery. If you have a laparoscopy, you will be admitted to a hospital and have a general anaesthetic for your procedure. Read our guide on preparing for surgery.
Laparoscopy is often used to treat gynaecological conditions such as endometriosis, to investigate infertility, if you need a hysterectomy, or for fibroids. It can also be used if you need surgery on your bowel or bladder. One of the main problems with open surgery (called a laparotomy, where a large cut is made in the tummy wall) is that recovery is slow and the wound is more painful. Studies have shown that following laparoscopy, your recovery is faster, you are back at home sooner and you have less pain than with laparotomy. But it is still a surgical procedure, so you will still need time to recover!
What happens when you have a laparoscopy?
If you are having a laparoscopy, your doctor will explain the procedure to you and you will be asked to sign a consent form that is specific for you. This will note the type of surgery you are having and is an opportunity for you to ask any questions that you may have about your procedure. The process of laparoscopy follows a number of steps. You can watch this video that will take you through the process of being admitted to the hospital for an endometriosis laparoscopy.
Patient Information - Laparoscopy
No matter which hospital in Australia you are attending, the basic steps are very similar and are as follows:
- Hospital registration
- Pre-operative ward
- The operating room
- Recovery and discharge
Hospital registration
During this first step, you will complete the necessary steps required by the hospital for your admission. This may be done online before you get to the hospital or by submission of admission papers. You should find out what time you need to arrive at the hospital and always plan for some extra time for any delays. Once the registration process is complete, you will be directed to the appropriate pre-operative ward.
Pre-operative ward
The pre-operative ward is where you will be prepared for your surgery. You will be checked into the ward by administration and or nursing staff. They will explain the next steps for you. They will ask you questions regarding your medical history, any allergies you have and any medications that you take. They will also check your vital signs such as pulse, blood pressure, body weight and temperature. It is important that you tell your doctor, the nursing staff and the anaesthetist of any medications that you are on (including over the counter medications without prescription and herbal medications). Your consent form will be checked with you and you will have the opportunity to ask any questions regarding your procedure.

The operating room
You will be transferred to the operating room when your surgery is ready to start. You will be taken to the operating room either walking accompanied by a nurse or on a hospital transfer trolley. You will be checked into the operating theatre by a nurse who will confirm your details with you. If you have walked to the operating room, you will be transferred to a hospital trolley and taken to the anaesthetic waiting area. Your anaesthetist will see you and put a drip in your arm and start fluids running into a vein. You will be moved into the operating room where you will be asked to move from the trolley to the operating bed. Monitoring devices for your heart and oxygen levels will be placed on you and the anaesthetic will begin with oxygen being given to you before you go to sleep.
People in the operating room will be your surgeon and assistant surgeon, your anaesthetist, a nursing team of (usually) three nurses, and the operating room assistant. Nursing or medical students may also be in attendance. Once you are asleep, your legs will be placed in padded supports. Your skin is cleaned with antiseptic solution from the thighs to the ribs and sterile drapes are placed over your entire body. A small incision is made inside the umbilicus (belly button) and this is the entry point that allows the telescope (laparoscope) to be inserted. Your tummy will be filled with gas to allow the organs and tissues to be seen. The entire abdomen from the under surface of the ribs (and the muscle called the diaphragm) all the way to the pelvis can be seen. The liver, stomach, large and small bowel as well as the outside of the uterus, tubes and ovaries can be seen. Only the outside of the bowel can be seen with a laparoscopy, so checking for other types of diseases or problems is not possible. You may need additional cuts in the tummy wall for more instruments. It may be only one additional cut or it may be 3 or more. Sometimes, all the operating is done through one slightly larger incision in the belly button. These second holes (called port sites) allow for other instruments to be used to move organs and perform the planned surgery.
When your surgery is complete, the instruments are removed, the gas is released and all the ports are taken out. Small cuts may not need any stitches at all. Larger cuts may have a deep stitch and one in the skin. You should check with your doctor if the stitches are dissolving or need to come out.
Recovery and discharge
Once your surgery is completed, you will be woken from the anaesthetic and taken to a recovery area. You may not remember much of this part of your surgery, since the effects of the anaesthetic are likely to impact your memory. This is normal and is due to the effects of the different medications given to you. In the recovery room, you will continue to be monitored and have your vital signs taken by nursing staff. You will usually spend between 30-60 minutes in the recovery room.
Once you are awake, your pain is under control and all your observations are stable, you will be returned to a post-operative area for further observation before being discharged if you are a day-stay patient, or will continue to be monitored if you are admitted to a post-operative ward for a longer time. You will usually be asked to empty your bladder, need to eat and drink, and have your pain managed with oral medications before you can be discharged. You will not be able to drive yourself home so someone should pick you up and be available to care for you following your surgery. Your doctor will provide specific post-operative instructions depending on your specific surgery. You are likely to experience discomfort in the following areas in the days after your surgery:
- At the wound sites
- In your pelvic area
- Under your ribs
- In your shoulder tips
This discomfort is usually mild and should get better over time. If there is no improvement after a few days, you should contact your doctor.
 Skip to main content
Skip to main content