Medications that contain hormones, such as contraceptives, limit the growth of the lining of the womb and can reduce pain and menstrual blood loss.
Not all aspects of pain associated with endometriosis respond to medications, for example, stabbing and aching pains can be from tight pelvic floor muscles and are best treated with pelvic floor muscle relaxation exercises. However, medications can be a useful pain management tool, and it is worth understanding when and why they are prescribed.

Hormone medications
Reduce pain by suppressing periods
Medications that contain hormones (the combined contraceptive pill or progestogen-only pills) limit the growth of the lining of the womb and can reduce pain and menstrual blood loss. These medications can be prescribed by your general practitioner, family planning specialist or your gynaecologist. Different pills suit different people and have different side effects. For example, if you have migraines, it is best to avoid pills that contain the hormone estrogen. Not all pills provide contraceptive cover, and some are subsidised by the pharmaceutical benefits scheme (PBS) in Australia, so it is best to consult your doctor to determine which one is best for you.
The combined oral contraceptive pill
If you are using the combined oral contraceptive pill (contains estrogen and progestogen), it is possible to reduce the number of periods you have by skipping the sugar pills and continuously taking active pills. For example, if you don’t take the sugar pills and only take active tablets every day for two pill packets, you will have a period every two months (6 times a year rather than 12 times a year).
Some people can reduce the number of periods they have in a year even further (if you have four periods a year you can have them in the school holidays) or take active tablets continuously without having a period, but others get spotting if they run too many pill packets together and have to take sugar tablets to have a period at regular intervals.
It is safe to limit the number of periods you have, and this will limit the number of pain triggering events (periods) you experience. Continuing the active tablets also means you can delay having a painful period if you have a special sporting or social event.

Progestogen-only pills
Progestogen-only (progestin) pills are available that are taken continuously to suppress periods (e.g. Visanne, Primulot). Some suppress ovulation and provide contraceptive cover, whereas others do not. Generally, progestogen-only pills have to be taken at the same time every day to be effective (especially for contraception) and suit people who are very reliable with pill taking and less concerned about contraceptive cover.
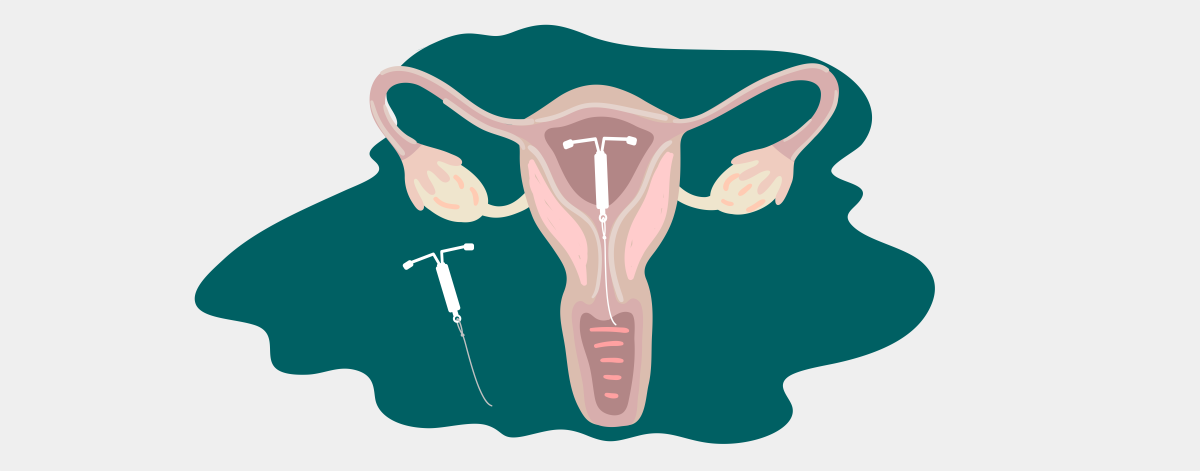
Implants and intrauterine contraceptive devices (IUDs)
Increasingly, people with endometriosis are choosing to use small implants that sit under the skin in the arm (Implanon) or in the womb (intrauterine contraceptive devices (IUDs) – Mirena, Kyleena) which continuously release progestogen to suppress periods.
These devices provide good contraceptive cover and after a few months of spotting, often result in no periods or very light monthly bleeds. Their side effects include ongoing spotting and hormonal changes like tender breasts and nausea, which generally settle over 4-6 months, so it is best to trial them for at least this long.
Some people with a sensitised pelvis find that intrauterine devices can trigger pain. Both devices can be removed in an outpatient setting and your fertility potential usually returns to normal within a month. These devices can be fitted by qualified general practitioners, family planning specialists and gynaecologists.
Additional resources
Medical management of endometriosis
Hormonal contraception and endometriosis
 Skip to main content
Skip to main content