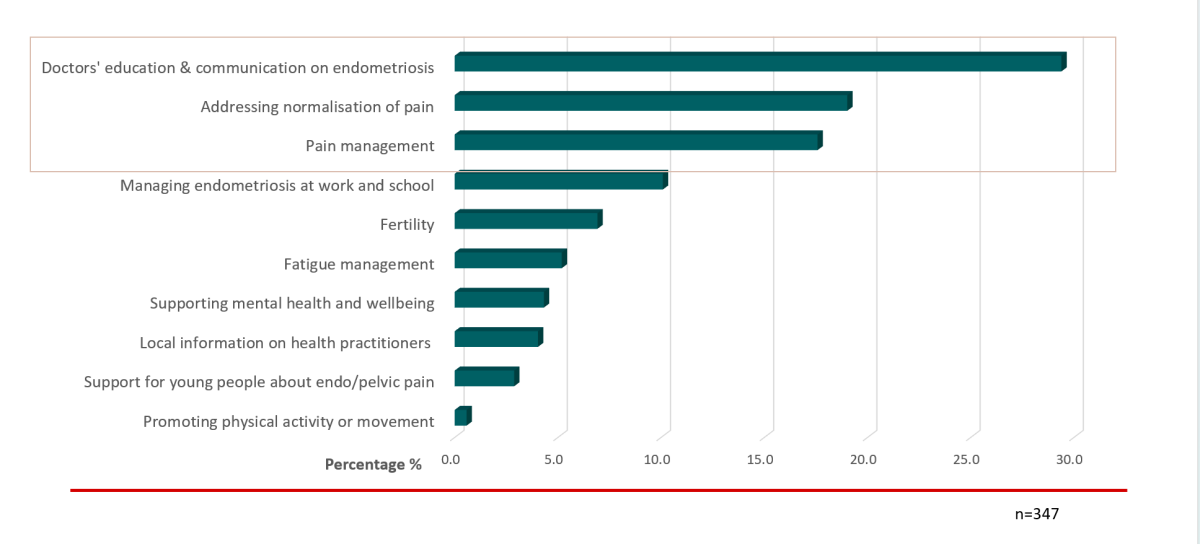
When we polled 347 community members as part of our research setting up this website, the highest priority (29%) for people with endometriosis was for better education about endometriosis.
In our focus groups, participants reported that health care providers can dismiss their symptoms, lacked knowledge of the condition and treatments, or inappropriately advocated pregnancy. EndoZone hopes to change this.
Quick links
Clinician resources
For many doctors, pelvic pain was covered in one or two lectures at medical school, which often focused on surgical treatment of endometriosis. We recognise that much has changed in this field and that many doctors would appreciate some support managing patients with pelvic pain. We understand that any information needs to be timely, quick to absorb and efficiently delivered in a busy clinical practice.
Quick facts about endometriosis
- 1 in 9 women and those assigned female at birth, are diagnosed with endometriosis in Australia
- On average patients have 8 co-morbid pain symptoms in addition to period pain
- Pelvic symptoms start early: 38% report their first symptom before 15; 66% before 20 years
- On average endometriosis patients lose 6.3 hours of work per week due to symptoms
- It takes 6.4 years to get a diagnosis of endometriosis from the onset of symptoms
- Endometriosis and pelvic pain costs Australia 7.4 billion dollars in direct and indirect health costs
- People with endometriosis are eligible for a chronic care plan
Why is it difficult to determine if pelvic pain symptoms are due to endometriosis?
This brief animation explains why pain symptoms don’t always correlate to anatomical lesions. Recurrent tissue breakdown and regeneration in endometriotic lesions create an inflammatory environment that activates the dorsal root ganglion in the back causing visceral, somatic and central pain sensitisation. There are many other pelvic pain triggers such as inflammatory bowel disease, chronic candidiasis, recurrent urinary tract infections, constipation and diarrhoea, mesenteric adenitis, interstitial cystitis, pelvic inflammatory disease and many more. These will activate the same pain response pathways and initiate a similar complex pain syndrome.
Understanding pain in endometriosis
Disclaimer: This is an area of evolving knowledge with ongoing research, this is what is currently understood about the condition at this time.
For the community version of this video (appropriate for patients) click here.
 Skip to main content
Skip to main content 








